Published estimates for the prevalence of breathlessness, medically known as dyspnea, in the general population vary between 9% to 59%, with a higher prevalence in older populations and in women. (Ref 1, Ref 2, Ref 3).
The prevalence of difficult intubation varies widely from 0.1% to 10.1% depending on the definition used (Ref 9, Ref 10). Difficult airway incidence during emergent intubation can be up to 10%, but complications of ICU airway management remain common. (Ref 4).
What is difficulty breathing?
Shortness of breath is when you feel like you can’t get enough air into your lungs.
It’s normal to sometimes feel short of breath, when you exercise or physically work hard, and your body needs more oxygen. Sometimes, difficulty breathing may be a sign of a health problem. (Ref 7).
What is a difficult airway?
A difficult airway is defined as the clinical situation in which a conventionally trained clinician experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both. The difficult airway represents a complex interaction between patient factors, the clinical setting, and the skills of the practitioner. (Ref 8)
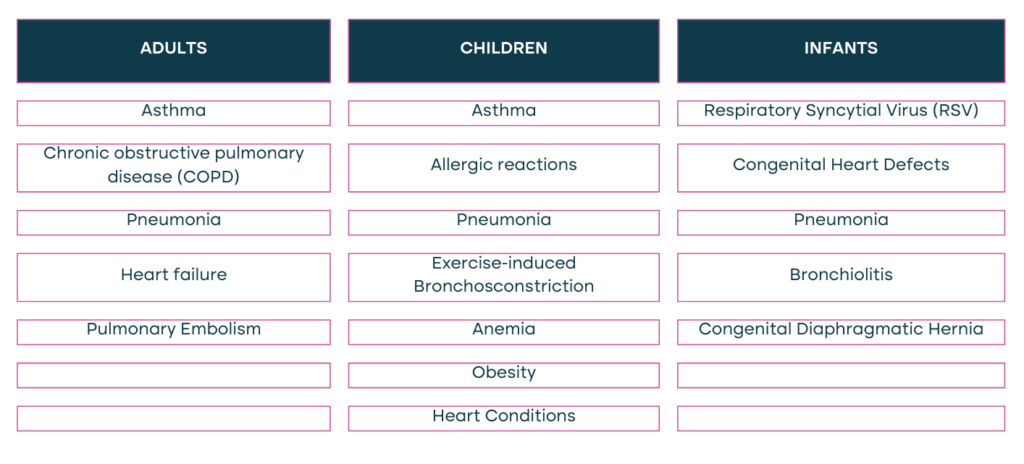
Difficulty in breathing can be caused by various factors:
Additionally, the factors below can contribute to a Difficult Airway:
- Anatomical Variations
- Limited user Experience
- Obesity
- Limited Mobility
- Facial Trauma or Burns
- Uncooperative or Agitated Patients
- Limited Access
- Radiation Therapy
- Scars and Previous Surgeries
- Pregnancy
- Congenital Syndromes
- Neck Masses or Tumours
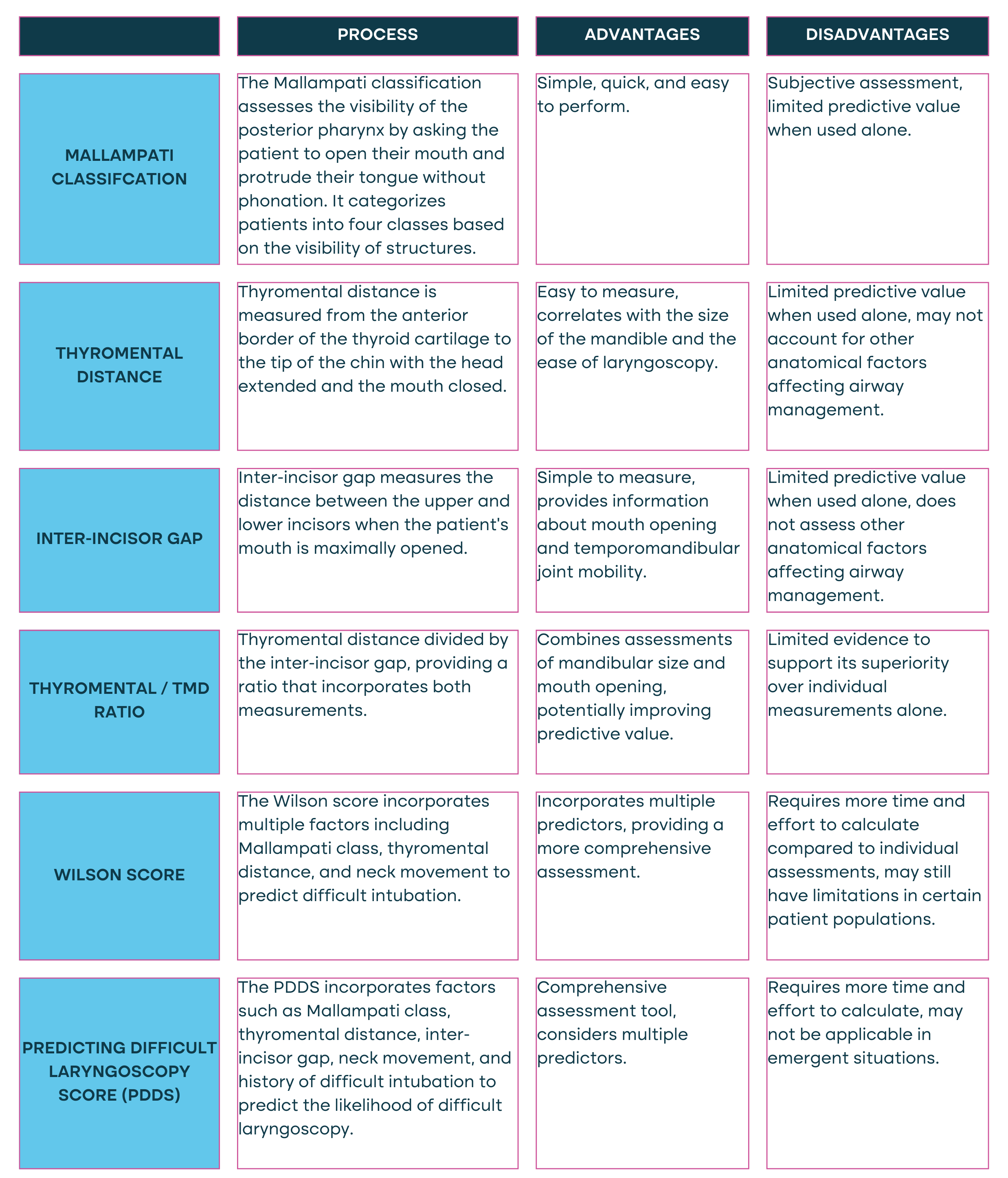
Evaluation of the airway for signs of potential difficulty should be performed as soon as possible on any patient in respiratory distress. Below outlines the approaches and processes which can be considered to assess and classify a difficult airway.
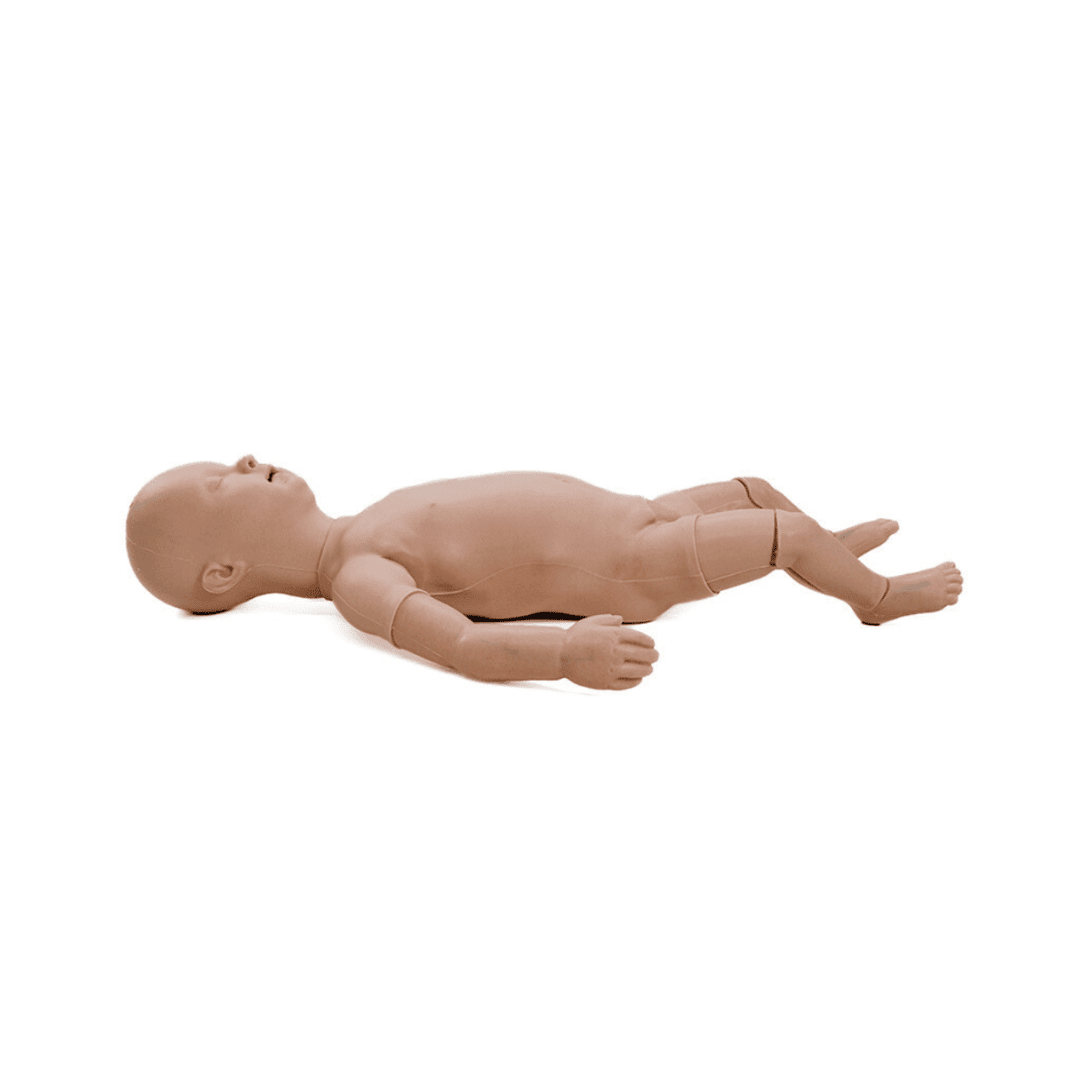
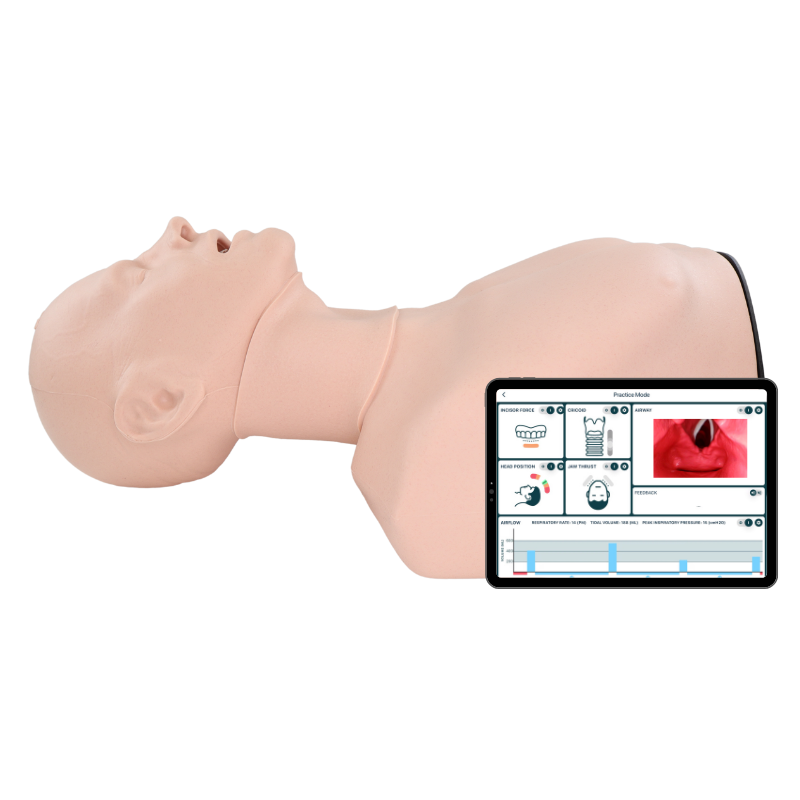
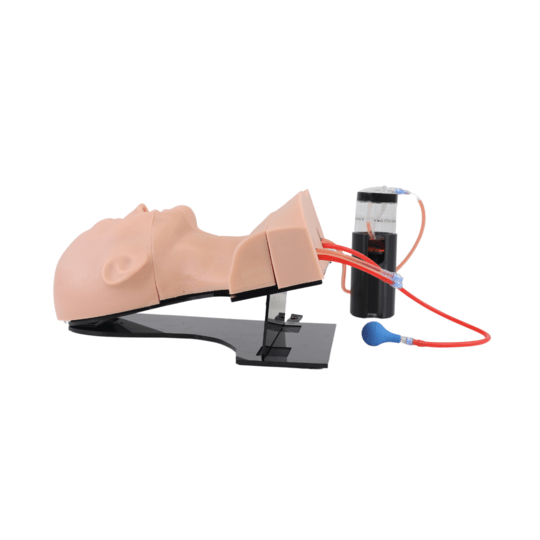
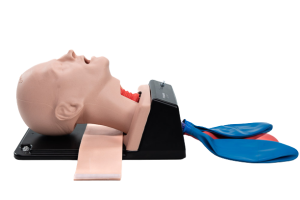
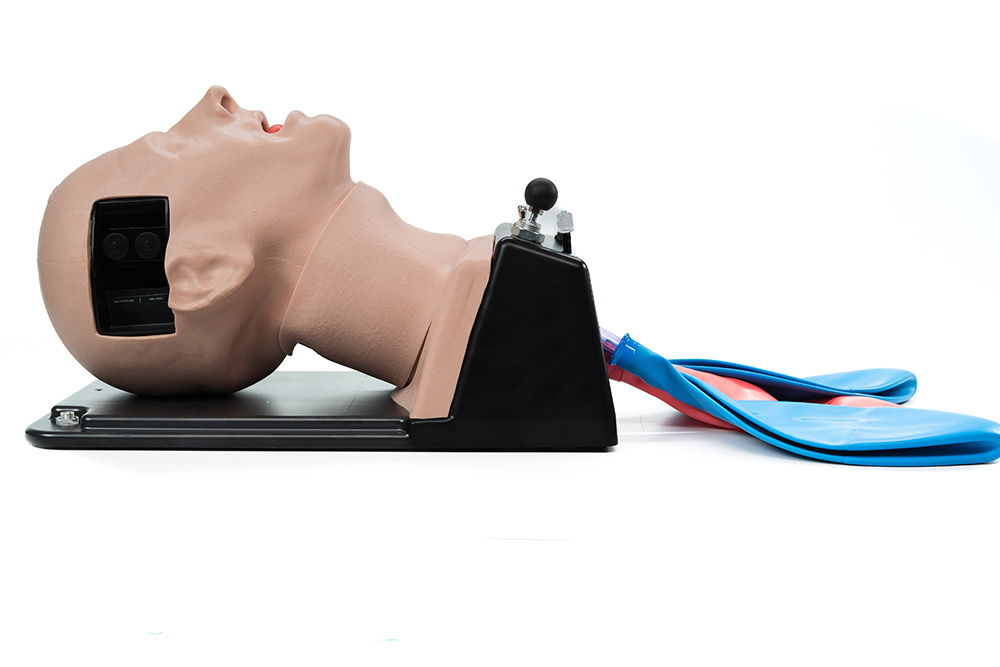
Manikin training and simulation enable development of technical as well as Non Technical Skills without subjecting patients to risk and allow multiple training sessions of relatively uncommon scenarios. (Ref 5).
TruCorp are proud to introduce the AirSim Difficult Airway trainer, an innovative approach to mastering airway management across a gradient of difficulties. The model has been designed for a wide array of users, extending from beginners to seasoned professionals, and is meticulously crafted to aid in the enhancement of skills required for managing unexpected, challenging intubations, in accordance with the Difficult Airway Society guidelines.
Medical Disclaimer for TruCorp Blog
- The information on the TruCorp blog is for educational purposes only and is not intended to replace professional medical advice or treatment. Always consult a qualified healthcare provider regarding any medical condition or treatment and do not disregard professional advice due to blog content.
- Content may not reflect the most current medical research and is not guaranteed to be error-free. TruCorp is not responsible for inaccuracies, nor does it endorse any specific medical procedures or products mentioned.
- Use of the TruCorp blog is at your own risk, and the company is not liable for any outcomes based on information provided. This disclaimer extends to comments from readers and contributions from guest authors.
- Always seek a doctor’s advice before making health changes. TruCorp is not liable for any damages from the use of information on the blog.
Source List:
1. Guenette JA, Jensen D, Webb KA, Ofir D, Raghavan N, O’Donnell DE. Sex differences in exertional dyspnea in patients with mild COPD: physiological mechanisms. Respir Physiol Neurobiol. 2011 Aug 15;177(3):218-27. doi: 10.1016/j.resp.2011.04.011. Epub 2011 Apr 16. PMID: 21524719. Sex differences in exertional dyspnea in patients with mild COPD: physiological mechanisms – PubMed (nih.gov)
2. Ofir D, Laveneziana P, Webb KA, Lam YM, O’Donnell DE. Sex differences in the perceived intensity of breathlessness during exercise with advancing age. J Appl Physiol (1985). 2008 Jun;104(6):1583-93. doi: 10.1152/japplphysiol.00079.2008. Epub 2008 Apr 24. PMID: 18436700. Sex differences in the perceived intensity of breathlessness during exercise with advancing age – PubMed (nih.gov)
3. Johnson MJ, Bland JM, Gahbauer EA, Ekström M, Sinnarajah A, Gill TM, Currow DC. Breathlessness in Elderly Adults During the Last Year of Life Sufficient to Restrict Activity: Prevalence, Pattern, and Associated Factors. J Am Geriatr Soc. 2016 Jan;64(1):73-80. doi: 10.1111/jgs.13865. PMID: 26782854; PMCID: PMC4719155. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4719155/#:~:text=Published%20estimates%20for%20the%20prevalence,older%20populations%20and%20in%20women.
4. Niven, Alexander S.a; Doerschug, Kevin C.b. Techniques for the difficult airway. Current Opinion in Critical Care 19(1):p 9-15, February 2013. | DOI: 10.1097/MCC.0b013e32835c6014 Techniques for the difficult airway : Current Opinion in Critical Care (lww.com)
5. Myatra, S.N., Kalkundre, R.S. and Divatia, J.V. (2017) ‘Optimizing education in difficult airway management’, Current Opinion in Anaesthesiology, 30(6), pp. 748–754. doi:10.1097/aco.0000000000000515. Optimizing education in difficult airway management: meeting the …: Ingenta Connect
6. Kollmeier BR, Boyette LC, Beecham GB, et al. Difficult Airway. [Updated 2023 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470224/
7. Shortness of breath (2023) healthdirect. Available at: https://www.healthdirect.gov.au/shortness-of-breath#:~:text=Shortness%20of%20breath%20is%20when,sign%20of%20a%20health%20problem. (Accessed: 29 March 2024).
8. Apfelbaum, J.L. et al. (2013) ‘Practice guidelines for management of the difficult airway’, Anesthesiology, 118(2), pp. 251–270. doi:10.1097/aln.0b013e31827773b2. https://pubs.asahq.org/anesthesiology/article/118/2/251/13535/Practice-Guidelines-for-Management-of-the
9. Rose DK, Cohen MM. The incidence of airway problems depends on the definition used. Can J Anaesth. 1996 Jan;43(1):30-4. doi: 10.1007/BF03015954. PMID: 8665631. The incidence of airway problems depends on the definition used – PubMed (nih.gov)
10. Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991 Dec;75(6):1087-110. doi: 10.1097/00000542-199112000-00021. Erratum in: Anesthesiology 1993 Jan;78(1):224. PMID: 1824555. Management of the difficult adult airway. With special emphasis on awake tracheal intubation – PubMed (nih.gov)
Meet the Writer:
Dr Ciaran McKenna is a full-time Consultant in Emergency Medicine practicing in the National health Service in Northern Ireland. He is also a HEMS Consultant with the Northern Ireland Air Ambulance in partnership with the Northern Ireland Ambulance Service.
Dr McKenna works alongside the team at TruCorp Ltd to develop innovative training solutions for the medical simulation industry, one of the most recent innovative product lines being TruCorp’s range of ultrasound task trainers.